Standard health care is vital for favouring and preserving health, preventing disease, and decreasing unwanted illnesses and early death.
Insurance is a procedure to purchase a protection plan based on particular loss, damage, disease, or death.The insurance service provider pays the money to the person who claims the policy.
Health care and insurance claims processing are integral to enhancing health services. This process assists customer satisfaction, enhances efficiency, and reduces costs.A prominent part of healthcare and insurance claim processing is an executive responsibility similarly crucial for good health care for patients.Health care and insurance claim processing can be available manually or digitally by subjecting claims through computerized data or online sites.
We will explore this content in healthcare & Insurance claims processing in detail.The factors that organise healthcare claims resolutions. The typical method of healthcare claims to strengthen the efficiency of processing.
But in reality, this method failed because of additional expenses.Eventually, a gradual trend of automation claims processing tools brings the potential to boost productivity and minimizes cost.
Advanced technology makes to be used to better and enhance the working process. A digitally claimed processing is relatively slow, but after a while, it will upgrade its functions.
The conflicts in healthcare claims processing
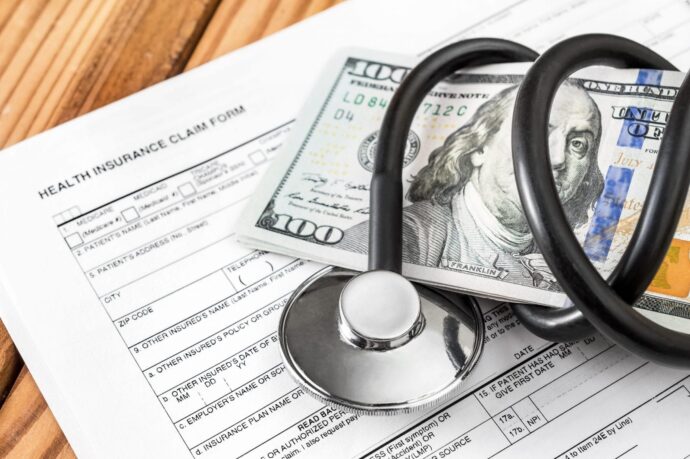
The claims process in healthcare and insurance needs massive statistics, including patients’ info, diagnosis by the doctor, testing record, insurance supplier data, payment info, and other essential information.
The data add manually demands a long time and the possibility of mistakes in the data. Here are the obstacles:
Medical Bills Errors: In the healthcare industry are studied as mistakes in patients’ names, incorrect product names, paying for twice, and a few others.
Linger in the claim process: Long hours influence healthcare service procedure.This process happened because of insufficient data and mistakes in the data submitted earlier.It will clash between the insurance provider and health care services.
Inadequacy of skilled persons: In this claim process, the inadequacy of qualified or trained persons should have followed and been aware of all the essential terms and guidelines.
Lacking to use current or latest medical code: Medical errors create a way toward claim rejection.
Wrong or mismatched data, using outdated code based on Current Procedural Terminology (CPT), International Classification of Diseases (ICD), and Healthcare Common Procedure Coding System (HCPCS) codes, create a high possibility of rejection. That requires an investigation and resubmission of data in this process.
Failure of communication: Failure of communication between health care services and insurance companies requires more appeals of claim services.
The procedures Healthcare & Insurance Claims Processing: To Improve Efficiency
There are several procedures to progress the health and insurance claims processing and improve efficiency.A combination of technology and AI (Artificial Intelligence) is a technique to boost efficiency in claim processing.
Developed medical software billing, along with adequate supervision, to boost efficiency in the healthcare sector.
Here are a few practical solutions:
Upgrade patient handling with automation
For the healthcare and insurance claim process, a smooth workflow is essential to take the right decision on time. Working on patient management, and enhancement in patients’ diagnoses, will bring efficiency to work.
No one is interested in being stuck in a claim rejection or failing to validate the data. Automation techniques lessen the labor cost and perform quickly and effectively.
Staff can find time to emphasize that they need more dedication and serve better for wellness. The automation process can validate mistakes, and the claims rejected will reduce data.
Voice assistance
The voice assistance or chatbot approach is an excellent way to deal with customers through the website or application. Chatbots can be used to guide by connecting with the policy owner to give a valid answer to their queries.
Only some customers prefer to connect with Chatbots or voice assistant features. But Chatbots can enhance the customer handing in a quick time.
Character Detection Technology
The technology can detect and validate data from the concerned person during a claim process is essential to access the services in due time.
Optical character recognition (OCR) technology is an effective solution for automating the info extracted from handwritten text or printed from a scanned-based document and transforming those text data to enable machine-readable format.
This process is a good way for the initial stage of claim processing and policy validation of claim processing.
So, in the initial stage claims and policy check procedure requires handwritten documents as valid proof. Policyholders’ statements, policies, and media info are essential documents.
In this way, OCR techniques can serve the role of data extraction of relevant information in the smooth processing of claim data.
Detection of Errors and Correction

In health care and insurance use of IT (Information technology) and healthcare automation software can detect errors while the claim stage also corrects the mistakes where done.
It is a significant way that catches errors and saves time in facing the struggle of claim rejection.
Immediate Notification and verify
Quick response technology like OTP (One time password) and quick mail after successful registration specific service.
Similarly, using any higher performance software that can notify the authority quickly. This technique can decrease the time to wait for long hours to get a confirmation of the claim processing.
The Aid of Computing technology
Computing technology or computer vision can evaluate costs and validate the relevant data from the image taken during the policy registration process.
The competing techniques can detect the data and certify those with the policyholder’s data thoroughly.
This process is a beneficial method to verify and validate the initial claim documents and has fewer chances of errors or false information.
A developed way for measuring service
A smartwatch displays the per day calories lost. Workout data, heart rate, and pulse rate are based on measuring the person’s body.
Similarly, advanced analytics or measuring tools can display utility info like the process claim investigation, policy checking, payment analysis, how the claim process works, or current status.
It can give time to time information about the claim process. The use of advanced measuring software can assist in informing about suspicious activities.
AI simplified workflow
In healthcare and insurance claim processing, AI technology can verify fraud identification, have less association with humans, and ease of service process for the claims.AI technology can validate particular policies, accurate code usage, and correct mistakes.
It can certify the policyholders’ essential data and proceed to the final stage after verification.AI technology saves time, minimizes human interaction, and decreases the health service and insurance policy validation process stepwise in less time than the regular handling of the claim process.
Use of a single tool to check essential message
Health care and insurance claim work notifications through text messages and email.It may be a point of worry to check and identify which is essential and which is not.Make use of a single communication tool that can notify about essential messages in a single platform.
Handling of data
Handing of entire data is an essential part of claim processing. Use essential data like verified copies and scanned documents and keep those files in any file management tool to get access to those files quickly when required.
If the file management process is not organized, it will create issues like wrong data submission, mismatch of documents, and delay in the claim process.
Superiority of Blockchain
The blessing of blockchain can assist with an enhanced solution in contrast to the regular way.It can provide the collocation of data and essential info using an intelligent way.
Blockchain can detect false claims and fraudulent data, notifying quickly through this technology. It enhances the directory authenticity process.
The digital health report is kept securely and brings more efficiency between the health care and insurance service process.
Take assistance from a professional service

In a few cases, healthcare organizations cannot supervise the top claim processing and lacing to provide sufficient time for systematic work processes.In this stage, research the professional service providers or consultancy dealing with similar service activities.
Connect with them, hire them to find solutions, and supervise those tricky parts with their expertise.
The benefits of health care claim
The benefits of health care claims enhance the claim management process in a quick time zone and enhance understanding of the upgrade way to get the solution.
Use AI, blockchain, the software tool to manage the work process effectively and reduce the workload.It decreases the claim time instead of waiting for a long duration.
It also minimizes the cost as compared with the regular processes. The usage of voice assistant features enhances customer service during the claim process.
Effective software solution
In the age of modern technology, effective healthcare claim software can supervise the workflow effectively 24/7.This software can assist in taking quick actions and solid solutions for the required services.
Examples: WayStar, Claim
Final Thoughts
Therefore, the content mentioned above is about healthcare & insurance claims processing: improving efficiency and automation can make a claim and work process more straightforward.
Using advanced technology, awareness of AI, blockchain and implementation will positively impact healthcare insurance efficiency.